You are the product of 37.2 trillion cells working together. Add the 100 trillion bacterial cells found in your intestines and skin, and you have 137.2 trillion cells that make you you. Each cell in your body converts the energy in carbohydrates and lipids (and sometimes proteins) into 10 million ATPs per second. That’s 3.72 x 1020 ATPs your body makes per second. (These numbers are averages. Some cells make more ATP than others, and ATP demand is in constant flux. Also, the amount of ATP produced by gut and skin bacteria is not part of the estimate.)
Metabolism occurs in all your cells. So, every organ in your body undergoes metabolism. However, some organs have a more significant influence on metabolism than others. In this chapter, we will be on five endocrine (hormone) organs that have a substantial impact on metabolism.
- Hypothalamus – releases hormones that stimulate the pituitary gland
- Pituitary gland – Releases the master hormones that stimulate the primary endocrine organs
- Pancreas – Release the hormones insulin and glucagon that regulate blood sugar
- Thyroid gland – Release thyroid hormone that stimulates a cells ability to use oxygen
- Adrenal gland – Releases hormones that regulate blood sugar, stress, inflammation, and protein catabolism
What is a Gland?
A gland is an organ but not all organs are glands?

An organ is “a group of tissues in a living organism that have been adapted to perform a specific function.” The heart, the liver, a muscle, a bone, and the salivary glands are organs. However, only the salivary glands are a gland.
Why?
A gland is an organ whose main function is secretion. The secretion can be body fluids (sweat and saliva) or hormones. The primary function of the salivary gland is to secrete saliva. The heart does secrete hormones, but its primary function is to pump blood.
The Pancreas
You are still an emergency room doctor. A patient arrives at the ER complaining about an unquenchable thirst and fatigue. They also complain about blurred vision, confusion, and nausea. You notice the patient has a fruity-smelling breath, a symptom of hyperglycemia. The patient’s urine test positive for glucose, which should not be in their urine. The patient’s blood glucose is at 185 mg/dL, 85mg/dL above normal. You suspect diabetes mellitus, so you order an insulin test.
Regulating Blood Glucose
The pancreas makes the majority of the digestive enzyme. It also makes the two primary hormones involved in blood sugar regulation. The Islet of Langerhans is a small section of the pancreas that contains the alpha cells and beta cells. Alpha cells secrete glucagon, a non-steroid hormone that raises blood sugar. Beta cells secrete insulin, a non-steroid hormone that decreases blood sugar. Insulin and glucagon are antagonistic hormones, which control the following negative feedback loop:
- When blood sugar rises above homeostasis (after eating), beta cells in the pancreas secrete insulin
- Insulin attaches to receptor proteins on adipose cells, liver cells, skeletal muscle fibers and “tells” glucose channel proteins to open
- Glucose leaves the blood and enters the cells
- When blood glucose reaches homeostasis, insulin secretion decreases
- When blood sugar drops below homeostasis (between meals), alpha cells in the pancreas secrete glucagon
- Glucagon attaches to receptor proteins on liver cells and “tells” the cells to break down glycogen into glucose.
- Glucose moves through channel proteins in the liver cells’ membranes and into the blood.
- When blood glucose reaches homeostasis, glucagon secretion decreases
Diabetes Mellitus: A Dysfunction in Regulating Blood Glucose
Type 1 diabetes is a disease in which the immune system destroys the beta cells of the pancreas. Without beta cells, there is no insulin. Without insulin, a person becomes hyperglycemic. But, the cells become hypoglycemic because they need insulin to get sugar. Without sugar, cells resort to using fat and protein as a source of energy. Without insulin treatment, organ failure and death will occur.
Type 2 diabetes also leads to a failure in blood sugar regulation. However, the cause of type 2 diabetes is diet and an inactive lifestyle. Type 2 diabetes is sometimes called insulin-resistant diabetes. A diet high in sugars and starches usually results in constant insulin secretion. Cells hyperstimulated by insulin will downregulate their insulin receptor proteins, or the receptors become desensitized to insulin. Over time, target cells become resistant to insulin, resulting in hyperglycemia. Also, the hypersecretion of insulin may lead to beta-cell atrophy.
The fruity smell on your patient’s breath is the result of elevated ketones. Ketones are an acidic product of fat catabolism. An increase in ketones can lead to acidosis, a life-threatening condition in which the body tissues become too acidic for enzyme function. The patient’s blood test indicates normal insulin and glucagon levels, a sign of healthy pancreatic function. Ruling the pancreas out, you set your sites on the thyroid gland.
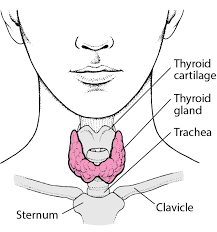
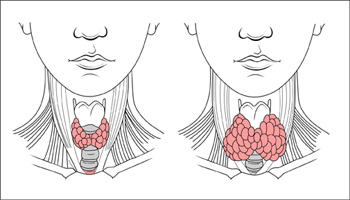
The Thyroid Gland
The thyroid gland is a butterfly-shaped organ found right below the Adam’s apple. It and the gonads (testes and ovaries) are the only endocrine organs adults don’t need to live. However, children with inactive thyroids have severe impairments in neurological and physiological development. Now, living without the thyroid is not all roses and chocolate-covered bees. A sluggish or lack of thyroid will result in a slowed metabolism, chills, lethargy, and weight gain. Those chocolate-covered bees may not be coming in the mail, but you are still alive.

Thyroid hormones are the only molecules in the body that contain iodine. The thyroid gland uses iodine to make the hormone thyroxine (T4). But, T4 has almost no effect on its target cells. T4 becomes an effective steroid when it loses an iodine atom and becomes the T3. T3 “tells” its target cells to increase oxygen usage, elevating the rate of aerobic respiration. Increased aerobic respiration leads to an increase in glucose catabolism (higher metabolism).

Hypothyroidism = decrease in T3 = Decrease in oxygen consumption by cells. Hyperthyroidism = increase in T3 = Increase in oxygen consumption by cells.
An inactive thyroid is a cause of hypothyroidism. Hypothyroidism leads to fatigue and weight gain. Your patient has lost weight, so an overactive thyroid is more likely. The symptoms of hyperthyroidism are like the symptoms of your patient. Yet, your patient’s blood tests show normal TSH levels, and T3 and T4, a sign of normal pituitary and thyroid function. Now, you wonder if the adrenal glands are the cause of the patient’s hyperglycemia.
The Adrenal Glands
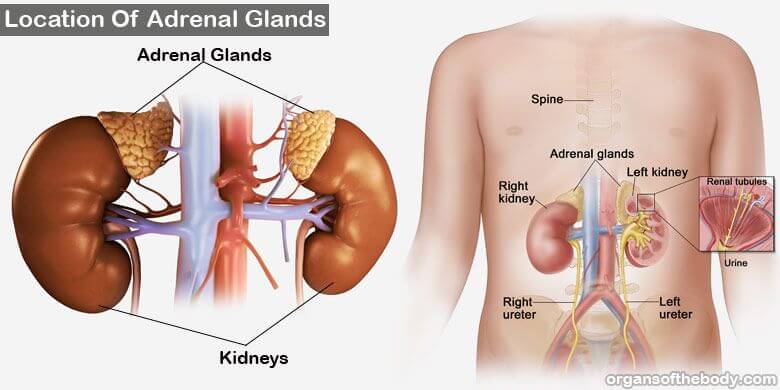
The adrenal glands sit on top of the kidneys like a hat on a skull. Adrenal hormones regulate libido, male sexual development, cell concentrations of water and salts, immunity, and metabolism. Cortisol is the principal adrenal steroid hormone involved in metabolism. Cortisol’s primary function is to prevent hypoglycemia. When blood sugar drops below homeostasis, cortisol “tells” its target cells to catabolize fats and proteins. Unlike glucagon, which targets liver cells, cortisol targets most cells of the body.
Epinephrine and norepinephrine are non-steroid adrenal hormones that also play a role in metabolism. Both hormones have a permissive effect on cortisol and a synergistic effect on glucagon to raise blood glucose. Epinephrine also has a permissive effect on T3 by increasing the aerobic catabolism of fat.
Epinephrine, norepinephrine, and cortisol are also known as the stress hormones released during the fight-or-flight response. The fight-or-flight response is also known as a sympathetic response because it triggers the nervous system’s active part. The sympathetic nervous system initiates a surge in all three adrenal hormones when exposed to a stressor. The rise in hormones preps the body to respond to the threat. However, a new study has found that the bone hormone osteocalcin may be the principal fight-or-flight hormone. In the study, one group of mice had their adrenal glands removed, preventing the secretion of cortisol and nor/epinephrine. To the researchers’ surprise, all the mice had a fight-or-flight response when exposed to stress. Another group of mice had functioning adrenal glands but were unable to secrete osteocalcin. Without osteocalcin, none of the mice produced a fight-or-flight response when exposed to stress. Whether these results are transferable to humans is not known. However, the study is another example of the complexities of human physiology.
Short-term stress is necessary for our bodies to respond to threats and exercise. But, chronic stress is harmful to the body. Sustained, elevated cortisol levels weaken the immune response and lead to muscle atrophy, anxiety, and sleep disruptions. One possible symptom of chronic stress is post-traumatic stress disorder (PTSD). PTSD is a condition in which a person’s exposure to an extreme stressor – e.g., war, abuse – produces a strong stress response. All future exposures to the stressor, no matter how small, can result in the same physiological response as the initial event. For example, a friend of my wife’s fought in Falluja during the height of the Iraq War. When our kids were toddlers, she had a straightforward request when attending parties: no balloons. Anytime a balloon popped, her body responded with a surge of hormones as it did during the Battle of Falluja. She may have been at a toddler’s birthday party, but her thoughts and physiology were at war.

After a few more tests, you discover that your patient has a tumor on their adrenal gland, causing the hypersecretion of cortisol. You recommend surgery for the removal of the abnormal cell mass.
.jpg)
Chapter Summary
- The pancreas makes the primary hormones that regulate blood sugar
- Beta cells secrete insulin when blood sugar rises after a meal rich in carbohydrates.
- Insulin attaches to receptor proteins on most cells’ membranes (liver, adipose, and muscle cells are the primary target cells), which tells the cells to take in glucose, lowering blood sugar.
- Alpha cells secrete glucagon when blood sugar drops between meals.
- Glucagon attaches to receptor proteins on liver cells and tells the cells to catabolize glycogen into glucose.
- The liver releases glucose, and there is an increase in blood sugar.
- Beta cells secrete insulin when blood sugar rises after a meal rich in carbohydrates.
- Type 1 diabetes is an autoimmune disorder where the immune system destroys the pancreas’ beta cells; therefore, a person needs supplemental insulin to regulate blood sugar.
- Lifestyle choices primarily cause type 2 diabetes. Target cells become less receptive to insulin, and insulin secretion may stop over time. Unlike type 1 diabetes, type 2 diabetes is reversible if treated in the early stages of the disease.
- The thyroid gland releases thyroid hormones (T3 and T4), which tell cells to use oxygen. Oxygen is required by cells to breakdown glucose and lipids into cellular energy (ATP).
- The adrenal glands secrete the hormone cortisol. Cortisol’s main function is to prevent hypoglycemia.
- The adrenal glands also secrete the hormone epinephrine, which has synergistic effects on glucagon by amplifying an increase in blood glucose.
- Epinephrine has a permissive effect on cortisol by increasing glucose uptake by cells.
- Cortisol, epinephrine, and the bone hormone osteocalcin are the primary hormones that trigger the fight-or-flight response.