You are an ER doctor. A patient arrives in the emergency room with the following physical symptoms: muscle cramps and spasms, facial twitching, muscle weakness, numbness in hands and feet, and bradycardia. The patient also had a seizure an hour before arriving at the ER, and he is confused, irritable, and anxious. You suspect hypocalcemia and ask the nurse to take a blood sample and send it to the lab for testing. While you are waiting for the lab results, you test for the Trousseau sign and Chvostek sign. The patient tests positive for both symptoms, a good indicator of hypocalcemia. The lab results show that the patient has deficient blood calcium levels, verifying hypocalcemia. Now you need to find the cause of his condition.
What’s So Why Do We Need Calcium
The cation calcium (Ca2+) might seem like nothing more than an atom that gave up two of its electrons, but this ion is essential for homeostasis. Calcium is involved in muscle contraction, neuron, and cardiac conduction, blood clotting, bone density and growth, and hormonal secretion. Without calcium, the symptoms your ER patient is showing will get worse, and if not corrected, it will lead to organ failure and death.
Bone stores calcium and releases it when needed. However, our most significant calcium source is in our food. Calcium can be found in large quantities in green leafy vegetables, dairy, chia seeds, salmon, sardines, almonds, beans, lentils, and fortified foods, to name a few. However, dietary calcium is only accessible when the body has enough vitamin D.
Vitamin D is a lipid-soluble molecule that originates from cholesterol. Very few foods contain vitamin D, so our primary source of Vitamin D is converting cholesterol in the skin to vitamin D via sunlight. (The physiology of vitamin D production will be discussed later in this chapter.)
Vitamin D has two primary calcium regulation functions:
- To facilitate the absorption of dietary calcium through the wall of the small intestine.
- To help regulate the deposition and removal of bone calcium.
Gross Anatomy of Bone
The 206 bones of your body come in five primary shapes:
- Long bones, such as the femur and radius
- Short bones, such as the carpals (wrist bones)
- Flat bones, such as the ribs and sternum
- Irregular bones, such as the scapula and vertebrae;
- Sesamoid bones, such as the patella (knee cap).
This chapter will focus on long bones since they are primarily involved in vertical growth.
Bone consists of spongy bone and compact bone. Spongy bone has many tiny spaces between a mesh of small bone fragments called trabeculae. The trabeculae act as cross beams that reduce bone mass without sacrificing strength. Compact bone is solid and does not contain trabeculae. Compact bone appears concrete with a few scattered holes where blood vessels enter and leave the bone marrow.
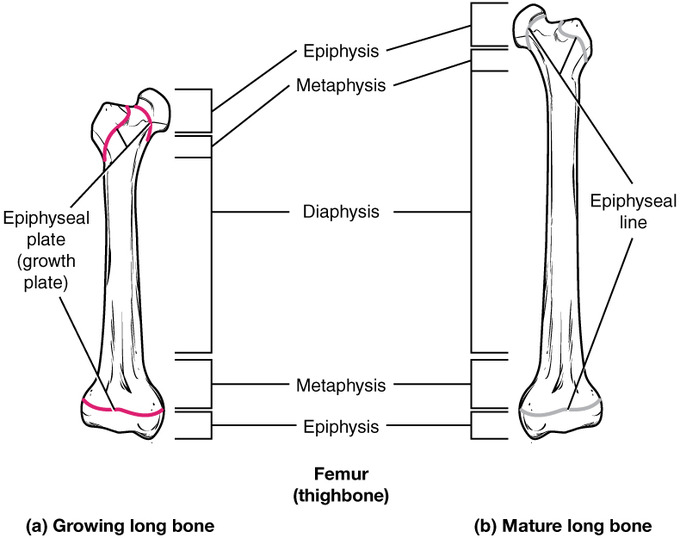
A long bone has two ends called the epiphyses and a shaft called the diaphysis. The epiphyses consist of spongy bone covered by a thin layer of compact bone. Hyaline cartilage covers the epiphyses’ ends, which aids in the smooth movement of movable articulations (joints). The diaphysis is a solid tube of compact bone with a chamber in the center that contains bone marrow.

Micro Anatomy of Bone
You are still an ER doctor. While working towards your bachelor’s degree, you worked part-time in construction, making concrete driveways and slabs for new houses. You learned that even though concrete has great compressive strength, it does not have high tensile strength. The addition of metal rebar makes an “endoskeleton,” and concrete is poured over it, reinforcing concrete.
Reinforced concrete is the go-to construction material of the modern era because it is lighter than almost all other structural materials. It is cheap, and it has high compression and tensile strength too.
For millions of years, nature has been using its form of reinforced concrete called bone. As you learned in Chapter 7, the extracellular matrix of bone consists of collagen fibers and the ground substance consisting of the crystal-like mineral hydroxyapatite (a calcium phosphate mixture). In bone, collagen fibers weave together, forming strong braids that act as “rebar,” giving bone high tensile strength.
The ground substance of bone consists of water, calcium, and phosphorus that form the “concrete” portion covering the collagen braids when mixed. Pound-for-pound bone has two times the compression strength of granite, is four times more resilient from stretching than concrete, and is stronger than steel of the same mass.
Bone contains three primary cells:
- Osteocytes maintain the bone matrix
- Osteoblasts build the bone matrix
- Osteoclasts break down the bone matrix and look and act similar to Metroids. (Metroids remove energy from their host, and osteoclasts remove calcium from bone.)
This chapter will focus on osteoblasts and osteocytes because they are the primary cells that maintain calcium homeostasis.
| These are Osteoclasts and Osteoblasts | This is a Metroid |
|---|---|
 |  |
Bone Remodeling
A common cause of hypocalcemia is tumor growths that affect the parathyroid gland. The parathyroid gland consists of four small dots on the thyroid gland’s lateral sides (two dots per side). Both the parathyroid and thyroid glands release hormones that maintain homeostatic levels of blood calcium.
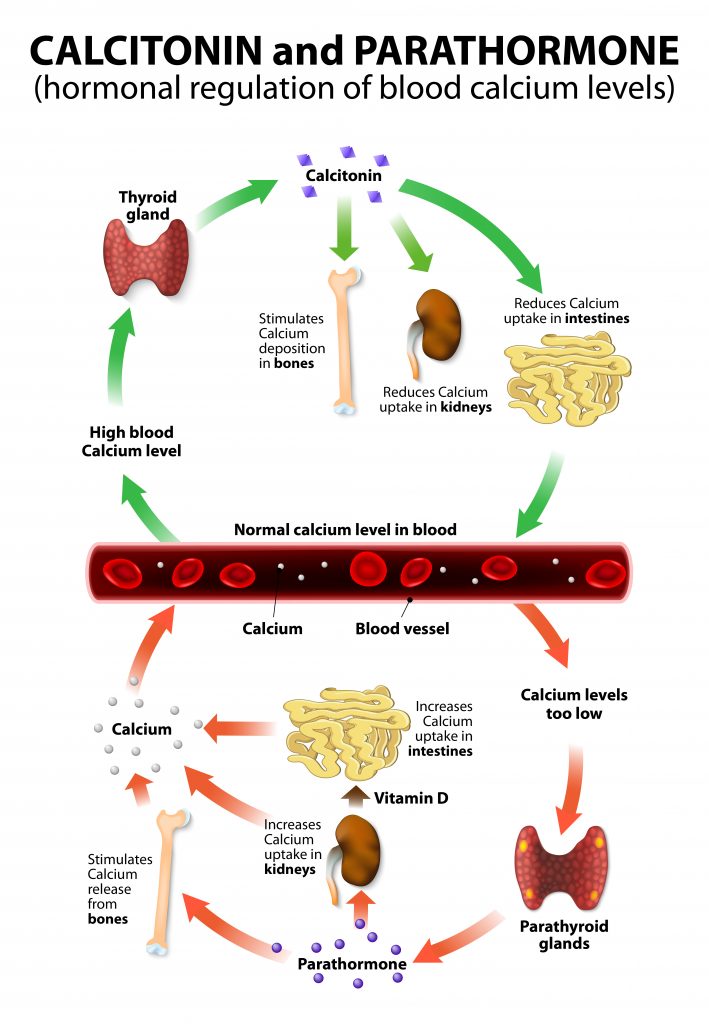
In a healthy individual, the parathyroid gland secretes parathyroid hormone, which activates osteoclasts. The osteoclasts break down the bone matrix, which releases calcium into the blood in bone resorption. When blood calcium levels reach homeostasis, the secretion of parathyroid hormone stops, and osteoclasts become inactive.
When blood calcium is too high, the thyroid gland releases the calcitonin hormone, inhibiting osteoclasts. Osteoblasts then use the extra calcium in the blood to build the bone matrix, a process called bone deposition. Once blood calcium drops to the body’s homeostatic set point, calcitonin secretion stops. Therefore, parathyroid hormone and calcitonin are antagonists that use negative feedback to maintain the calcium homeostatic setpoint.
After a series of tests, your patient’s parathyroid hormone levels are normal, but his vitamin D levels are deficient. You now turn your sights on the kidney and small intestine.
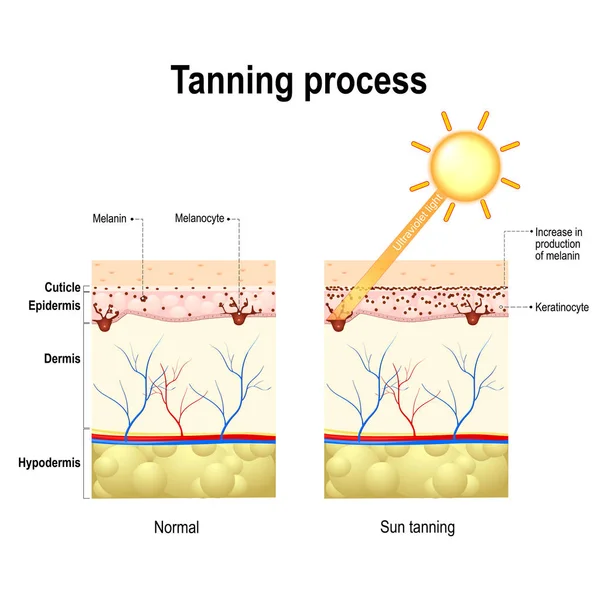
Cholesterol + Sunlight = Vitamin D
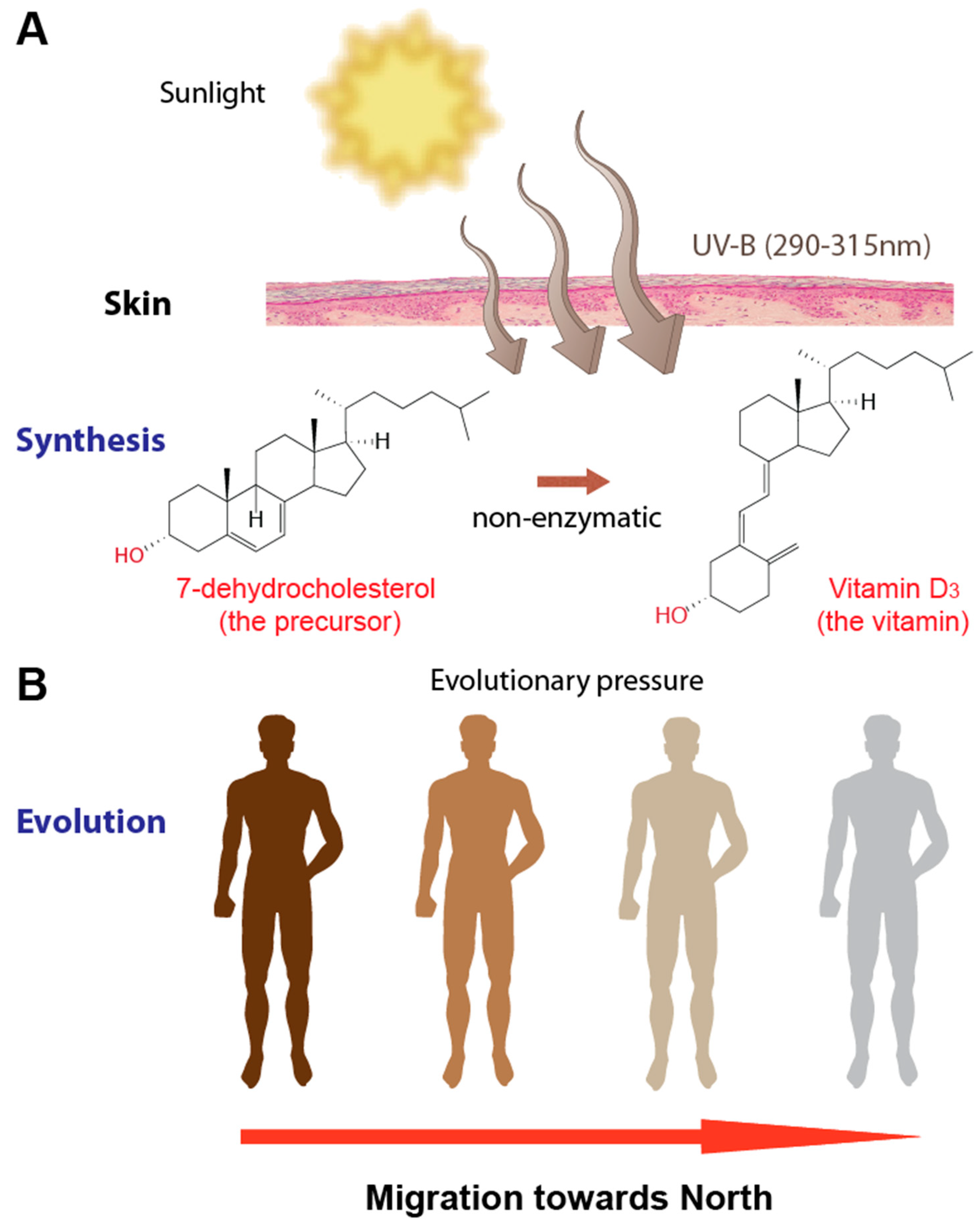
Two hundred thousand years ago, in East Africa, a new population of humans became Homo sapiens. The first sapiens had dark hair, irises, and skin, which benefited those living in sun-intensive East Africa. One hundred fifty thousand years later, modern humans arrived in Northern and Eastern Europe, regions with lower light intensity. A few modern humans were born with a mutation that instructed their melanocytes (a type of skin cell) to produce less melanin (pigment in the skin). Lighter skin is a disadvantage in sun-intensive regions of the globe because less melanin means less protection from ultraviolet (UV) radiation. However, lighter skin has an advantage in Europe because sunlight is not as intense, decreasing vitamin D production. Over thousands of years, Europeans’ skin pigmentation became lighter and lighter the farther north they went, allowing them to make vitamin D in areas of the globe where there is less yearly sunlight.
So what does this brief history lesson on modern human evolution have to do with calcium regulation? The answer is two-fold:
- The environment selects which phenotypes (traits) increase the chances of survival
- Until vitamin D fortification, humans’ primary vitamin D source was exposure to UV radiation.
Therefore, protection from the harmful effects of UV radiation and UV radiation’s use to convert cholesterol into vitamin D are selection pressures. Dark skin has an advantage at lower latitudes but is a disadvantage at higher latitudes. And vice versa for light skin.
The physiology of vitamin D production is complex, so here are the key points:
- UV radiation converts cholesterol in the skin to pre-vitamin D3.
- The liver converts vitamin D3 into the hormone Calcidol
- The kidneys convert Calcidol into vitamin D
- Kidneys store vitamin D
Here is the calcium regulation negative feedback process simplified:
- When blood calcium levels are low, the parathyroid gland releases parathyroid hormone (PTH), and bone resorption begins:
- osteoclasts to break down bone, which releases calcium into the blood
- kidneys reabsorb (move into the blood) calcium from the solution that will become urine
- kidneys release stored vitamin D
- Vitamin D allows the small intestine to absorb calcium into the blood
- When blood calcium rises to homeostatic levels, PTH secretion slows
- When blood calcium levels are too high, the thyroid gland releases calcitonin, and bone deposition begins
- Inhibits osteoclasts, which increase bone deposition by osteoblasts
- Tells kidneys not to reabsorb as much calcium (more calcium in the urine)
- When blood calcium returns to homeostatic levels, calcitonin secretion slows
So, in short, no vitamin D = calcium in the food will not be absorbed by the body = hypocalcemia = symptoms of your patient.
After asking your patient about his diet and lifestyle, you discover that he is agoraphobic, allergic to dairy, and hates vegetables and seafood. Therefore, his diet and lack of exposure to natural light likely caused hypocalcemia.
You administer intravenous calcium gluconate until his blood calcium reaches homeostasis and prescribe oral calcium and vitamin D.
Please Don’t Use Tanning Beds
So, are tanning beds a great way to increase my vitamin D?
No. Using a tanning bed is one of the worst things you can do to your body. The high-intensity UV radiation emitted from tanning beds accelerates aging and increases the risk of skin cancer. Using a tanning bed once can increase a person’s chances of getting malignant melanoma (the deadliest type of skin cancer) by 20%.
How about if I apply sunscreen before I use a tanning bed?
What? No. No one should use a tanning bed. Period.
Let’s say I convert my bed into a tanning bed and then cover my body with a blanket and apply sunscreen to the blanket. Will this make a tanning bed safe?
I wonder if Target is highering.
Vertical Bone Growth
You were born with about 300 bones, and by the time you stop vertical growth, you will have 206 bones. How did you lose nearly 100 bones in less than two decades?
Alien abduction?
What? No!
A close encounter of the fourth kind?
That’s alien abduction!!!!!
So it is alien abduction.
No!!!!!! It is not alien abduction! The answer is growth plates!
So, aliens abduct our growth plates?
Hello, Target. Yeah, I’ll take any position. . .
The epiphyseal plate, or growth plate, is a hyaline cartilage layer that separates the epiphyses from the diaphysis in long bones. The growth plates continue to grow and produce new bone until the cessation of vertical growth.
Here is how chondrocytes and osteoblast build new bone longitudinally:
- Near the epiphysis, chondrocytes build the cartilaginous matrix, which thickens the epiphyseal plate
- Near the diaphysis, the cartilage ages, and blood vessels (primarily capillaries) begin to penetrate it
- Via the capillaries, osteoblasts enter the cartilaginous matrix and convert it into bone
- The diaphysis of the bone grows vertically (longitudinally)
Vertical growth will continue as long as cartilage production keeps pace with ossification (new bone). Once cartilage production stops and the epiphyses and diaphysis meet, vertical growth stops forever. What is left is a “scar,” known as the epiphyseal line.
| This is the Epiphyseal Plate | This is the Epiphyseal Line | This is Gerald |
|---|---|---|
 |  |

Endocrine (Hormone) Control of Vertical Growth
The hormones released from the pituitary gland, liver, and gonads (testes and ovaries) are the primary hormones involved in vertical growth. Here is a simplified step-by-step explanation of the negative feedback loop that governs vertical growth:
- The hypothalamus releases growth hormone-release hormone (GHRH)
- GHRH stimulates the anterior pituitary gland to release human growth hormone (hGH) into the blood
- Via blood vessels, hGH moves to the liver and stimulates the production of the hormone, insulin-like growth factor-1 (IGF-1)
- IGF-1 enters the blood and moves to the epiphyseal plates within long bones and “tells” chondrocytes to make more cartilage.
- When blood IGF-1 rises above homeostatic levels, it inhibits the hypothalamus and pituitary gland from releasing more hGH, which slows the production of IGF-1.
- The release of hGH and IGF-1 will also stimulate skeletal muscle growth, so muscles grow in proportion to the bones.

Sex Hormones and Vertical Growth
Testosterone and estrogen increase the secretion rate of human growth hormone, and insulin growth factor-1 causes the speed of ossification to outpace cartilage production. A few years after puberty, the epiphyseal plates disappear, and the epiphyses bond to the diaphysis for the first time. The complete fusion of bone signals the end of vertical growth and the beginning of the 206-bone adult skeleton.
Bone Density
Our bones reach their peak density in our 20s through our early 30s. Our peak muscle density occurs during the same time frame. During this decade, our muscles exert a lot of force on the bones, to which the bones respond by increasing their density. However, when our muscles begin to atrophy (get smaller), they exert less force on the bones; therefore, bone density decreases.
By the time we reach our late 30s to early 40s, our bone density begins to decline. Males have a slow but steady decline in bone density, while females have a faster and greater bone density loss. Since women have less bone mass, the rapid loss of bone density is why women are more likely to develop osteoporosis.
Osteoporosis is a degenerative bone disease that leads to the loss of bone density. Women are more likely to get osteoporosis because they have lower bone densities and, after menopause, estrogen levels plummet. Estrogen reigns in osteoclasts, and without the hormone, osteoclast function will increase, increasing the bone atrophy rate.
The best treatment for osteoporosis is prevention. Males and females should get at least thirty minutes of exercise daily and eat a diet rich in calcium and vitamin D. Other treatments include estrogen therapy, medication, and possible surgery to strengthen brittle bone.
Calculating Bone Density
Bone density less than 833 mg/cm3 is at a greater risk of fracture. Below is one of the scales doctors use to determine if a patient needs treatment:
Osteopenia is sometimes referred to as “pre-osteoporosis.” Most females over the age of 50 and men over the age of 55 have osteopenia. In short, it is a condition every one of us will eventually get.
Doctors use Long bones, such as the femur, to calculate bone density. Since the diaphysis of long bones is a cylinder, clinicians use the formula for the area of a cylinder.
Example #1
A 1.25 cm3 sample of bone weighs 950 mg. What is the patient’s bone density?
Formula: Density = mass / volume
Density = 950 mg / 1.25 cm3 = 760 mg/cm3
This patient has osteopenia.
Example #2
What is the bone density if the length of the diaphysis sample is 10.0cm, the diameter is 2.5cm, and the mass of the sample is 47g (47,000mg)?
The formula for volume of a cylinder: Volume = πr2h
Volume = 3.14(1.56 cm2)(10cm) = 49 cm3
Density = 47,000 mg / 49 cm3 = 959 mg/cm3
This patient has normal bone density.
Chapter Summary
- Bones store calcium
- Bone resorption: When blood calcium levels drop below homeostasis, the parathyroid gland releases parathyroid hormone (PTH). PTH stimulates osteoclasts to break down the bone matrix, which releases calcium into the blood.
- Bone deposition: When blood calcium levels rise above homeostasis, the thyroid gland releases calcitonin. Calcitonin inhibits osteoclast function, which allows osteoblasts to remove calcium from the blood to build bone density.
- Vitamin D production
- UV radiation from the sun stimulates the conversation of cholesterol to pre-vitamin D3 in the skin.
- The liver converts vitamin D3 into Calcidol
- The kidneys convert Calcidol into vitamin D and store it
- Vitamin D and calcium regulation
- When blood calcium drops below homeostasis, PTH stimulates
- osteoclasts to breakdown the bone matrix
- kidneys to release vitamin D
- Vitamin D allows the small intestine to absorb calcium in food.
- When blood calcium levels rise above homeostasis, calcitonin
- inhibits osteoclasts, allowing osteoblasts to deposit calcium into the bone matrix
- Decrease the reabsorption of calcium by the kidneys – i.e., more calcium in the urine
- When blood calcium drops below homeostasis, PTH stimulates
- Vertical growth happens at the epiphyseal plates (growth plates)
- Hyaline cartilage is replaced by bone, lengthening the bones.
- Human growth hormone
- The hypothalamus stimulates the pituitary gland to secrete human growth hormone (hGH)
- hGH stimulates the growth of the epiphyseal plates
- hGH stimulates the secretion of IGF-1 by the liver
- hGH and IGF-1 are synergistic and work together to speed up vertical growth
- Osteoporosis and osteopenia are conditions resulting in the loss of bone density, particularly the spongy bone (a decrease in the number of trabeculae)




![The distribution scheme of mineral elements in bone matrix [2]; cF:... | Download Scientific Diagram](https://www.researchgate.net/profile/Artem_Semenov/publication/288686621/figure/fig1/AS:330401513000962@1455785267311/The-distribution-scheme-of-mineral-elements-in-bone-matrix-2-cF-collagen-fibril.png)