Review of Nephron Anatomy
Filtration
About every 45 minutes, the nephrons filter your entire volume of blood plasma. Filtration occurs between a tangled cluster of capillaries called the glomerulus and the Bowman’s capsule (aka glomerular capsule). The glomerular capillaries contain large fenestrae (holes) through which hydrostatic pressure pushes some blood plasma (~20%). The leaked plasma is a slurry of water and solutes (electrolytes and nonelectrolytes) small enough to squeeze through the capillaries’ holes. Water, glucose, H+, K+, urea, creatinine, NaCl, and amino acids are a part of the plasma slurry, but blood cells, platelets, and proteins remain in the blood because they are too large to fit through the fenestrae. The plasma solution filters through the Bowman’s capsule and enters the renal tube (the tubular portion of a nephron). The plasma is now called the glomerular filtration fraction, or the filtrate.
Hydrostatic pressure is the force that pushes the filtration fraction (filtrate) out of the glomerular capillaries and through the Bowman’s capsule’s membrane. However, there are two opposing forces affecting filtration. Proteins are too large to leave the blood and are nonpermeable (nonpenetrating) substances. The blood becomes hypertonic as the filtration fraction (filtrate) leaves the glomerulus. Some of the filtration fraction moves back into the capillaries via the osmotic gradient – a force called blood colloid osmotic pressure, which is osmotic pressure. The second opposing force is the hydrostatic pressure of the filtrate in the glomerular capsule. Yeah, that’s right, hydrostatic pressure is a two-way street. So, what do you get when you combine all three of these forces?
The Triforce?
No. It’s the net filtration pressure.
Triforce is a much better name.
True, but that name has a copyright, and it doesn’t explain glomerular filtration.
It could.
How.
Princess Zelda and Link are the filtrate’s osmotic pressure and hydrostatic pressure that fight against the evil hydrostatic pressure of the blood, Ganon!
Well, in the kidney, the blood’s hydrostatic pressure is greater than the combined osmotic pressure and filtrate’s hydrostatic pressure. Therefore, Ganon wins.
Well, Link and Zelda had a good run. Sometimes the evil pig wins.
Anyway, there is a formula for calculating the net filtration fraction:
Hydrostatic pressure in the glomerular capillaries (HPg) – osmotic pressure (OPg) – hydrostatic pressure in the Bowman’s capsule (HPbc) = net filtration fraction (Pnet)
HPg – OPg – HPbc = Pnet
Let’s do a sample problem:
The hydrostatic pressure in the glomerular capillaries (HPg) is 55 mmHg, the osmotic pressure in the glomerular capillaries (OPg) is 30 mmHg, and the hydrostatic pressure in the filtrate (HPbc) is 15 mmHg. What is the net filtration rate (Pnet)?
55 mmHg – 30 mmHg – 15 mmHg = 10 mmHg is the Pnet

Sample Problems to Solve Filtration Rate
In statistical analysis, percentages are written in decimal form. For example, 100% is written as 1.0, and 8.2% is written as 0.082. You will be using statistical nomenclature to solve for filtration fraction and renal blood flow. Therefore, you must convert percentages (72.8%) into statistical form (0.728).
Calculating Daily Urine Volume
Bob Bobby is a healthy adult that filters 185 L of blood plasma per day. However, 99.2% of the filtered plasma is reabsorbed into the blood. Therefore, how much urine in liters does he excrete per day?
Formula: Total Urine Volume: (Total volume of plasma filtered per day) x (% of plasma not reabsorbed)
First, find the percentage of the filtrate that is NOT reabsorbed back into the blood (the percentage urinated).
1.0 – 0.992 = 0.008
Now calculate the urine volume:
185 L x 0.008 = 1.48 L of urine per day
Calculating Blood Plasma Volume
Pete Petie Peterson weighs 73 kg and has a blood volume of about 8% of his body weight. What is his whole blood volume? If we assume his blood plasma is 56% of his total blood volume. What is his plasma volume?
Formula: body weight x (% blood weight x % of blood plasma) = Plasma volume in liters.
73 kg x 1 L/ 1 kg x (0.08 x 0.56) = 3.37 liters of blood plasma
His kidneys filter 180 L of plasma per day. How many times does he filter his total plasma volume?
Formula: Total liters filtered per day/liters of blood plasma
180 L / 3.37 L = 53.4 times per day
Calculating Filtration Fraction
Frank Frankie weighs 62 kg. Assuming that his total blood volume is 7% of his body weight, his heart pumps his total blood volume once a minute, and his renal blood flow is 25% of the total blood volume per minute. Calculate the volume of blood in liters that flows through Frank Frankie’s kidneys each minute.
Formula: Volume of Renal Blood Flow per minute = (weight in kg x % of blood volume) x % of total blood volume to kidneys per minute
(62 kg x 1 L/ 1 kg x 0.07%) x 0.25 = 1.08 L/min
57% of his total blood volume is plasma. Calculate the amount of blood plasma filtered each minute
1.08 L/min x 0.57 = 0.62 L/min
Filtration fraction is the percentage of blood plasma filtered at the glomerular capsule, which is 20%. Calculate his filtration fraction in liters per minute.
0.62 L/min x 0.20 = 0.124 L/min
=
How?
It’s. . . beautiful.
All accurate graphs are.
Reabsorption
Before calculating the filtration rate, we need to discuss how 99% of the filtered blood plasm is put back into the blood. There are a plethora of solutes small enough to leave the glomerulus and enter the nephron. However, we will focus on seven of them. They are glucose, amino acids, NaCl, H+, K+, urea, and creatinine.
Surround the nephron is a web of capillaries that will collect the reabsorbed filtrate.
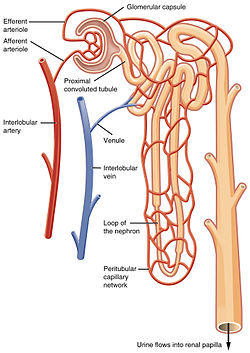
Reabsorption begins along the walls of the proximal convoluted tubule (PCT). Simple cuboidal epithelium lines the PCT walls, and the cells have microvilli on their free surface to ensure maximum absorption of the filtrate. Most reabsorption occurs here.
- All of the glucose and amino acids reabsorb via active transport.
- Some NaCl reabsorbs via active transport
- Most of the water, K+, and urea reabsorb via passive transport.
- H+ and creatinine are NOT reabsorbed.
The remaining filtrate moves along the loop of Henle. The first half of the loop of Henle is the descending limb because it moves downward. Only water and urea passively reabsorb through the descending limb walls.
At the bottom of the loop of Henle, the reaming filtrate moves up the ascending limb. NaCl passively and actively reabsorbs back into the blood.
Secretion
Secretion is the process of removing excess creatinine, H+, and K+ from the blood plasma. Creatinine passively secretes through the PCT walls. If the blood is too acidic, H+ ions actively secrete into the DCT. And, if the hormone aldosterone is present, the Na+/K+ pump actively secretes K+ into the DCT and collection duct.
Here’s a table of where and how water and the seven solutes reabsorb and secrete along the nephron.

Excretion
The final filtrate is urine. Urine is collected in the kidney’s renal pelvis, exits via the ureters, and travels to be stored in the urinary bladder. Urine leaves the urinary bladder through the urethra during micturition (urination).
