A Brief Overview of Immunity
The First Line of Defense: The Skin and Mucous Membranes
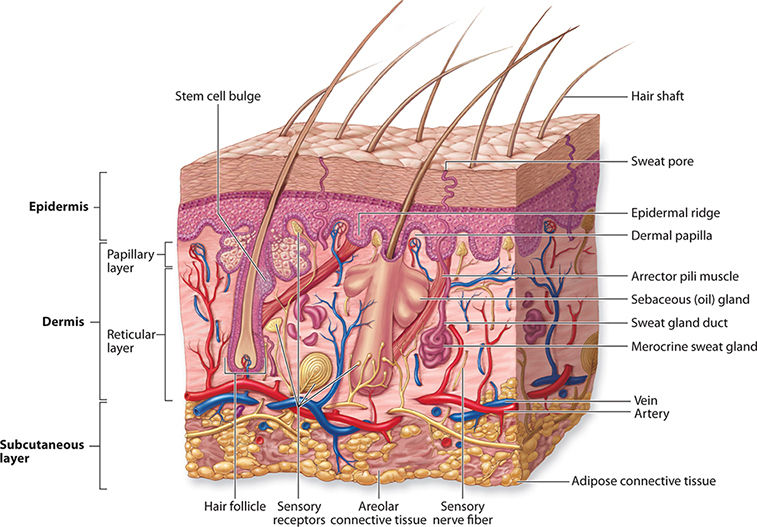
The skin comprises eight percent of your body mass and, until recently, was considered to be the human body’s largest organ. The skin is a two-layer multifunctional organ. The epidermis is the avascular superficial layer comprising keratinized stratified squamous epithelium, and it has multiple functions:
- A water-resistant layer that regulates the amount of water in and out of our bodies
- An antimicrobial layer that keeps pathogens at bay
- Absorbs harmful UV radiation
The dermis is the skin layer deep to the epidermis. The dermis is a vascular layer about twice as thick as the epidermis and contains the hair follicles, sebaceous (oil) glands, and sudoriferous (sweat) glands. The sebaceous glands secrete the oil sebum, which lubricates the skin and increases its water-resistant properties. Sudoriferous glands secrete sweat, which cools the body and releases metabolic waste.
The skin is our first line of defense against pathogens by acting as a near-impenetrable barrier and is home to the second-largest microbiome. The skin biome is essential for healthy skin and the innate and acquired immune responses.
Our bodies also contain several orifices such as the mouth, nasal cavity, ears, and urethra. Each one of these openings secretes solutions that ward off pathogens. For example, saliva in the mouth and mucus in the nasal cavity contains a slurry of enzymes and antimicrobials that kill contagions.
The Second Line of Defense: Innate Immunity
Contagions that make it past our first line of defense will encounter our innate immune system. The innate immune system comprises a series of responses that will attack any foreign antigen, which is why it is also called nonspecific immunity. The nonspecific immune response’s effects produce the symptoms common in most infections: inflammation, fever, and nausea.
The innate immune system gets its name because it is fully functional at birth. The acquired or adaptive immune response is not fully functional at birth and needs to “learn” how to fight infections throughout a person’s life. For example, you are born with a brain and almost all the neurons you will ever have (innate immune system). Still, your brain must continually make and break synapses as it processes and learns from the sensory information it receives (acquired immunity).

Cytokines are hormone-like chemicals secreted primarily by leukocytes that modulate the immune response (also called interleukins). For example, pyrogens are a class of fever-inducing cytokines. The elevated temperature or fever makes it easier for phagocytes and natural killer cells to attack pathogens, and the high temperature usually weakens the contagion. Our hypothalamus and monocytes (macrophages and dendritic cells) release pyrogens when exposed to an antigen. The number of pyrogens released correlates to the increase in body temperature. In most situations, the rise in body temperature is within the homeostatic range, so we do not develop a fever. However, fever develops when the antigen poses a significant threat to the body. Children are more likely to have higher fevers than adults when exposed to the same pathogen because their immune systems are still learning to react to foreign antigens.
Interferons are a group of cytokines released during a viral infection. Interferons warn cells of a viral invader, and they “tell” infect cells how to fight the virus or commit apoptosis.
Inflammation is one of the first innate responses during infection and injury. Basophils and mast cells are the two primary leukocytes responsible for inflammation. Basophils and mast cells initiate inflammation using different physiological pathways, but understanding these differences requires a more in-depth explanation of innate immunity that is more appropriate for a college-level physiology class (if you’d like to know the differences, click here). So, for simplicity, we will consider mast cells and basophils the same white blood cell. When tissue is damaged or a foreign antigen enters the body, basophils secrete the chemical histamine, starting inflammation. During inflammation, the following occurs:
- The fenestrae in capillary walls get larger, allowing more blood plasma and white blood cells to enter the infected/damaged tissue
- The inflamed area warms, increasing the effectiveness of healing and immunity.
- Neutrophils and macrophages phagocytize bacteria
Inflammation is necessary for a proper immune response, but too much inflammation is problematic. Excessive inflammation can lead to elevated blood pressure, edema (swelling of tissues), joint pain, restricted airflow, and hypovolemic shock, to name a few. A diet rich in saturated fat and sugar will lead to chronic inflammation, increasing the likelihood of type II diabetes and heart disease.

Natural Killer (NK) cells are cytotoxic lymphocytes that kill cancer cells and viral-infected cells. NK cells are not antigen-specific because they can kill most cancer types and cells infected with most viral types. NK cells are the first cytotoxic T cells at the infection site and will remain until the immune system makes enough cytotoxic T cells.

The Last Line of Defense: Acquired Immunity
Acquired immunity takes the longest to respond to a foreign antigen, but it will produce the most robust and lethal response. B and T lymphocytes are antigen-specific and must acquire the ability to kill their target pathogen. Therefore, B and T cells can only respond to and attack one specific antigen. For example, SARS-CoV-2 (the COVID-19 virus) B and T cells will only attack the coronavirus or cells infected with the coronavirus.

Macrophages and Dendritic Cells
Macrophages and Dendritic cells are a part of the innate immune system because they will phagocytize any foreign antigen. However, these two phagocytes play an essential role in initiating acquired immunity. After a macrophage or dendritic cell eats a pathogen, it places the contagion’s antigen in its cell membrane, luring a helper T cell to it, and acquired immunity begins.

Antibody-Mediated Immunity
All white blood cells are born from hematopoietic stem cells in the red bone marrow. However, the location of lymphocyte maturation determines its nomenclature. B cells mature in the bone marrow, and T cells mature in the thymus.
B cells differentiate into plasma cells or memory B cells. Plasma cells secrete antigen-specific proteins called antibodies. Each unique plasma cell and its clones can only produce antibodies for one specific antigen. You will make billions of different antibodies throughout your lifetime; therefore, you will make billions of different B cells.
Antibody-mediated immunity occurs in a series of steps that start with exposure to an antigen and ends with the production of antibodies that attack said antigen. Here are the major steps:
- Antigen-bearing pathogens enter tissues
- A dendritic cell or macrophage phagocytizes the pathogen and displays the pathogen’s antigen on its cell membrane
- Helper T cells become activated as they recognize the antigen on the macrophage’s membrane
- Helper T cells secrete cytokines which stimulate the B cells that make the complement antibody (an antibody that attaches to the foreign antigen)
- B cells make clones of themselves, creating plasma cells
- Plasma cells release antibodies into the blood plasma, which destroys extracellular pathogens or marks infected cells.
- When there is systemic destruction of the contagion
- Regulatory T cells tell most of the remaining plasma cells to commit apoptosis
- Memory B cells remain in circulation and quickly destroy the pathogen with the same antigen if it reenters the body
It is important to note that antibodies can only attach pathogens outside of cells. The acquired immune response creates cytotoxic T cells that kill infected cells.

Cell-Mediated Immunity
T cells mature in the thymus. The thymus is an organ superior to the heart that is teaming with T cells ready to govern the acquired immune response (helper T cells) or kill virally infected cells (cytotoxic T cells).
Helper T cells are the generals of the immune system. When they encounter a foreign antigen on a macrophage, they immediately search out and activate B cells and cytotoxic T cells with the complement receptor protein (a receptor protein that matches the antigen’s shape). T cells differentiate into memory T cells and cytotoxic T cells. The cytotoxic T cells quickly make clones that will seek out cells infected with the antigen.
Here are the steps to cell-mediated immunity:
- An infected cell will display a virus’ antigen on its membrane
- Macrophages or dendritic cells activate helper T cell
- Helper T cells activate cytotoxic T cells (killer T cell) and “teaches” them how to recognize the foreign antigen
- The cytotoxic T cells attach to the virus-infected cells and inject a cytokine into the infected cell that causes it to commit apoptosis.

Achieving Immunity
Most contagions we encounter we become immune to. However, it takes at least one exposure to an antigen to gain immunity against it.
Primary Immunity
Primary immunity is the acquired immune system’s response to the first exposure to an antigen. It usually takes the body 7-10 days to produce enough antibodies and cytotoxic T cells to exterminate the contagion. If an antigen causes disease, then it can reproduce fast enough to cause symptoms. If a person remains asymptomatic of a pathogen, it usually means that they produce enough B and T cells to stop the pathogen from spreading. (However, being asymptomatic does not always mean a person is not sick. Some people are asymptomatic for COVID-19 and end up on a ventilator.)
At the end of primary immunity, regulatory T cells tell most plasma cells and cytotoxic T cells to commit apoptosis. However, memory B and T cells remain in the blood and circulate for years. The second time you are exposed to the same antigen, your memory B and T cells will initiate the secondary immune response.
Secondary Immunity
When memory B and T cells come in contact with a known antigen, they initiate a rapid and powerful secondary immune response. The secondary immune response rapidly produces a very large army of plasma B cells and cytotoxic T cells. The response usually happens within a day, and the amount of B and T cells produced is many times that of the primary immune response. Therefore, the secondary immune response usually eradicates the contagion before it can harm the body and cause disease symptoms.


Passive and Active Immunity
Passive immunity is when a person receives antibodies from a vaccine or another person, and these antibodies fight off infections. However, the antibodies do not stimulate the person’s immune system, so they will not produce B and T cells that fight off the pathogen. Once the antibodies are broken down, passive immunity ends. If a person is exposed to the pathogen again, they will begin primary immunity.
Active Immunity is when a person receives a vaccine that contains a death pathogen or a severely weakened pathogen. This will stimulate the production of B and T cells and will simulate the primary immune response. If a person is infected with the pathogen in the future, they will automatically enter the secondary immune response.
