Heart Development
The heart is the first functional organ to develop in utero. Eighteen days after fertilization, a single cell begins to beat. That cell multiplies into two cells and those two cells divide and become four cells. The cell division is so rapid that it takes three days for the heart to start pumping blood.
Your heart develops and remains in the center of your thoracic cavity between the lungs. Its primary function is to pump blood through the blood vessels to most of the body’s tissues. The heart continuously beats until the heart muscle no longer functions. The body’s tissues and organs cannot get oxygen and nutrients when it stops. Death quickly follows.
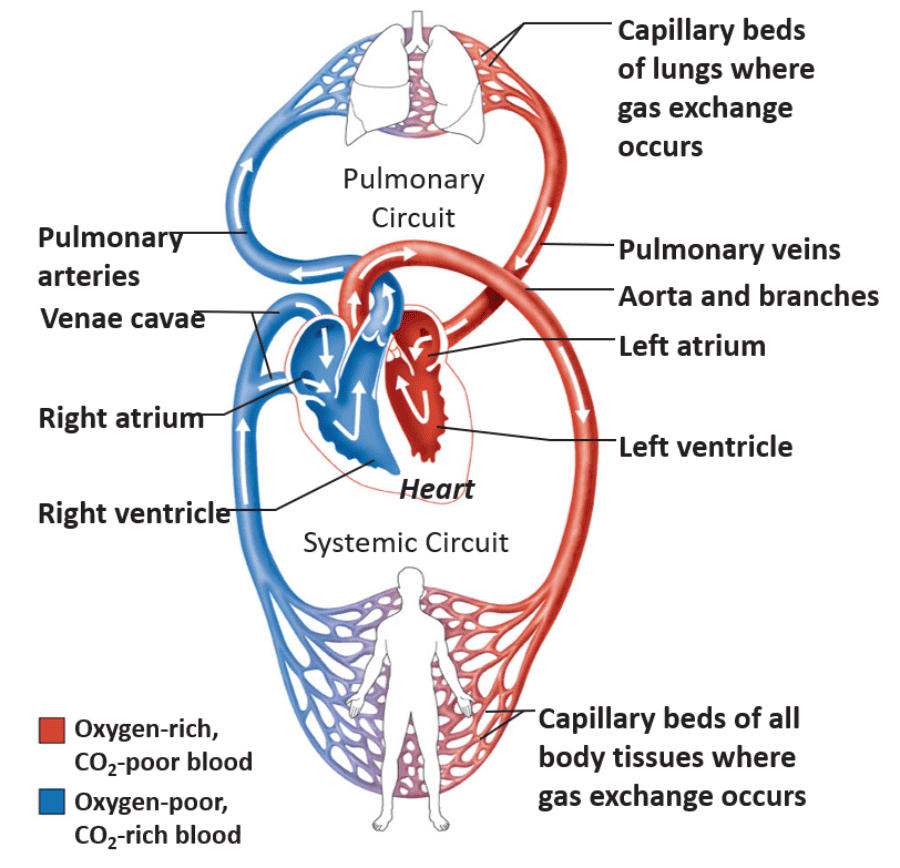
Blood Circulation
There are three primary types of blood circulation:
- Pulmonary circulation includes the arteries moving toward the lungs, the capillary beds within the lungs, and the veins returning blood from the lungs to the heart.
- Systemic circulation comprises the arteries moving to all of the body’s tissues (except the inner lungs and heart), all the capillary beds within the body’s tissues, and all of the veins returning the blood to the heart.
- Coronary circulation refers to the heart’s arteries, capillaries, and veins.
Blood Vessels
Blood vessels are the roadways of the body. You have about 100,000 miles of blood vessels in the body with a diameter ranging from a quarter to a single strand of hair. There are three primary types of blood vessels in your body. Arteries take blood away from the heart. Veins carry blood toward the heart. And the movement of water, gasses, and nutrients happens through the capillaries’ walls.
A common misunderstanding is that arteries are larger than veins. Arterial walls are twice as thick as the walls of veins; however, a vein’s lumen, the inner space containing the blood, is five times larger than arterial lumens. Capillaries have the smallest lumen and thinnest walls of the blood vessels.

Arteries
Arteries take blood away from the heart and move it toward the body’s tissues. The heart pumps blood into the arteries; therefore, the blood pressure is highest in the arteries. Arteries’ walls are thick, elastic, and muscular, which can withstand dynamic pressure changes. For example, an adult’s average resting blood pressure is 110/70 mmHg (an mmHg is a unit for pressure). The higher number, 110 mmHg, is the systolic blood pressure, which is the pressure against the arteries’ walls when the heart contracts. The lower number, 70 mmHg, is the diastolic blood pressure, which is the pressure against the arteries’ walls when the heart relaxes. The arteries of a person with a resting blood pressure of 110/70 mmHg experience a 57 percent change in blood pressure between heart relaxation and contraction. During exercise, the difference in blood pressure between heart contraction and heart relaxation can be greater than 100 percent.

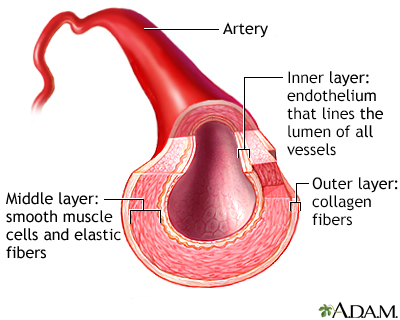
Arterioles
Arteries get smaller as they move away from the heart. Once the arteries lose their continuous surrounding smooth muscle layer, they become arterioles. Arterioles have smooth muscle patches that regulate the capillaries’ blood pressure. For example, in the kidneys, there are clusters of capillaries where the blood is filtered. The blood filtration rate needs to be constant. However, arterial blood pressure is in perpetual flux. The arterioles in the kidney keep blood pressure consistent through vasoconstriction and vasodilation. Arteriole vasoconstriction happens when the blood pressure is above homeostasis and reduces the renal capillaries’ blood pressure, decreasing filtration. The arterioles vasodilate when the blood pressure is below homeostasis, increasing the blood pressure in the renal capillaries and filtration.


Capillaries
When the arterioles shed their smooth muscle, they become capillaries. Capillaries are tubes formed from a layer of simple squamous epithelium called the endothelium. Dotting the endothelium, are tiny holes called fenestrae. The size and number of fenestrae depend on the location of the capillaries. For example, the fenestrae in the kidneys are large so filtration can happen fast. However, brain capillaries do not have fenestrae because what enters and leaves the brain is tightly regulated.


Capillaries have the smallest lumen, but they have the greatest surface area. The high surface area increases the rate of diffusion through their thin walls. Simple squamous epithelium comprises the capillary walls, ensuring fast gas exchange between the blood and body tissues, and the blood and the lungs.
About 5-10% of your capillaries contain blood because there is not enough blood to fill all of the capillaries. Precapillary sphincter muscles regulate the blood flow through capillary beds. For example, food digestion happens while resting. The precapillary sphincters to the digestive organs’ capillaries are open, ensuring adequate blood flow. However, when your teacher releases pterodactyls into the room (one of the labs in this unit), the digestive precapillary sphincters close, and the precapillary sphincters to the skeletal muscles open. The rerouting of blood flow ensures your muscles have the oxygen and nutrient supply needed to tame the pterodactyls (such a fun and educational lab).

Venules
Capillaries become venules when the endothelium gains a layer of fibrous connective tissue. Venules are tiny veins that take blood from the capillaries to the veins. Once a thin layer of smooth muscle surrounds the venules, they become veins.
Veins
Veins move blood toward the heart. Veins have the largest lumens, but their walls are thinner than arteries. The veins have almost no blood pressure, so they do not have thick, muscular walls. Gravity primarily moves the blood in the veins superior to the heart. Veins inferior to the heart push the blood via skeletal muscle contractions.
The veins below the heart contain valves. When skeletal muscles contract, they squeeze the veins, which pump the blood toward the heart. However, gravity pulls the blood toward the feet when the muscles relax. The one-way valves within the veins prevent blood from pooling in the lower extremities.


Heart Structure
The heart has four chambers. The two upper chambers are the left and right atria, receiving blood from the veins. The two lower chambers are the left and right ventricles, which pump blood into the arteries.
The interventricular septum is a muscular wall separating the right and left heart chambers. The left ventricle is larger and contains more cardiac muscle in its walls compared to the right ventricle. The left ventricle needs the extra muscle to pump blood to all the body tissues (systemic circulation). The right ventricle does not need as much muscle because it pumps blood to the lungs (pulmonary circulation).
The atrioventricular valves (A-V valves) separate the atria from the ventricles. The tricuspid A-V valve separates the right atrium from the right ventricle. The name tricuspid refers to the three cusps that comprise the valve. Tendons called the chordae tendineae connect each cusp to a spire-like papillary muscle extending from the ventricular wall. The bicuspid A-V valve (mitral valve) has two cusps and separates the left atrium from the left ventricle. The bicuspid valve also connects to papillary muscles via the chordae tendineae.

The semilunar valves partition the ventricles from the arteries they pump the blood into. The valves’ cusps look like the moon in one of its earlier stages, hence their name. The pulmonary semilunar valve separates the right ventricle from the pulmonary artery, and the aortic semilunar valve separates the left ventricle from the aorta.
The primary function of the heart valves is to ensure blood flows in one direction through the heart. The closure of the A-V valves stops the blood from reentering the atria when the ventricles contract. When the ventricles relax, the semilunar valves’ closure prevents the blood from returning to the ventricles.

Blood Flow Through the Heart
Blood below the heart returns via the inferior vena cava vein, and blood above the heart returns via the superior vena cava vein. The blood in the vena cava veins has very little oxygen and high carbon dioxide levels.
The deoxygenated blood enters the right atrium and then moves through the tricuspid valve into the right ventricle. The right ventricle pumps the deoxygenated blood through the pulmonary semilunar valve into the pulmonary arteries. The pulmonary arteries are the only arteries that carry oxygen-poor blood. The deoxygenated blood flows to the lung capillaries, where carbon dioxide leaves the blood and oxygen enters the blood. The oxygenated blood flows back to the heart via the pulmonary veins – the only ones carrying oxygen-rich blood. The oxygenated blood flows into the left atrium and then through the bicuspid (mitral) valve into the left ventricle. The left ventricle pumps the oxygen-rich blood through the aortic semilunar valve into the aorta. The blood flows to the systemic capillaries and then returns to the heart via the veins.

At rest, the blood will move through both the blood vessels of the pulmonary circulation and systemic circulation in a minute. Therefore, a resting heart rate of 68 beats per minute means it takes 68 heartbeats to move the blood to and from the heart in one minute.