A Scenario
You are an emergency room doctor – it’s been a few chapters since I have done this shtick, so bear with me. A patient with a knife wound in his right thoracic wall arrives at the ER. You observe that the patient’s trachea deviates to the right and has difficulty breathing. Using a stethoscope, you hear asymmetrical breath sounds indicating a collapsed lung. The patient also has a deep wound on the left lateral side of the thoracic cavity. You suspect that the patient is suffering from pneumothorax and order a chest x-ray to confirm your diagnosis.
Pulmonary Respiration (aka Pulmonary Ventilation)
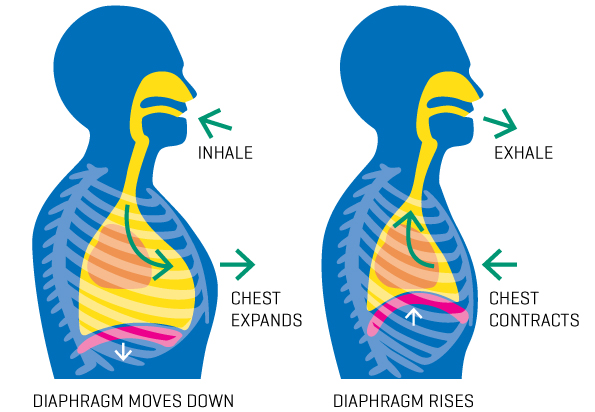
At rest, you take about 17 breaths per minute. A breath, or one respiration, begins with inspiration. When discussing breathing, inspiration means inhaling, not encouraging – though you should encourage yourself to breathe. (Ha. Ha. Ha.) When you inspire, the diaphragm contracts and moves downward. The diaphragm is a thin skeletal muscle that separates the thoracic and abdominal cavities, and its movement is essential for pulmonary respiration. The diaphragm’s downward movement increases the thoracic cavity volume, which causes lung pressure to become less than the atmospheric pressure. Air naturally wants to follow its pressure gradient, so the air enters your nasal and oral cavities and then moves into the pharynx, the back of the throat. The air then moves through the larynx, or voice box, into the trachea.

Rings of hyaline cartilage support the trachea and prevent it from collapsing. The mucus secreted by goblet cells in the ciliated pseudostratified columnar epithelium lining the trachea traps impurities and pathogens from the air. The cilia move the contaminants out of the respiratory tract.


Radom Vaping, Cigarettes, Marijuana, and Hard Drugs Fact
What do vaping and smoking cigarettes, marijuana, and hard drugs such as cocaine have in common? Well, if you answered with an increase in respiratory disease and cancer of the respiratory tract, you’d be right.
Vaping and smoking paralyze and kill the cilia that line your trachea and bronchial tubes. Without mobile cilia, pathogens and carcinogens remain in the respiratory tract, leading to pneumonia, emphysema, and cancer. Oh, and vaping and smoking accelerate the aging of the skin, decrease life expectancy and quality of life, and increase the likelihood of impotence.
The trachea forks at its distal end, and the air enters your right and left lungs via the bronchial tubes. The bronchial tubes branch into a labyrinth of smaller and smaller bronchial tubes known as the bronchial tree. At the end of the bronchia tree, the smallest tubes, called bronchial ducts, lead to the final destination, the alveoli.


Your heart sits in the center of your thoracic cavity between two lungs. Due to liver placement, the right lung is broader, thicker, and shorter than the left because the diaphragm is higher on the right side. The left lung has a notch in its medial side because the apex of the heart veers to the left. Each lung partitions into lobes, with the right lung having three lobes and the left lung having two lobes.

Expiration begins when the diaphragm relaxes and moves upwards. The diaphragm’s upward movement decreases the thoracic cavity volume and increases the pressure within the lungs. The increased pressure forces the air out of the lungs through the bronchial tubes, then the air moves through the trachea, larynx, and pharynx and exits the body via the nasal and oral cavities.

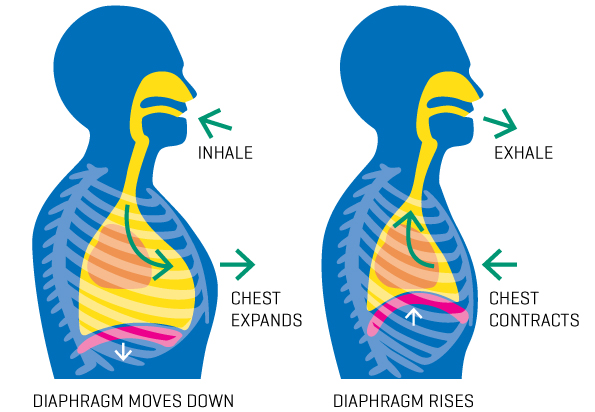

Here are some epic GIFs of inspiration and expiration.


Lung Volumes
The volume of air that moves during respiration depends on how much oxygen the body requires. The tidal volume (TV) is the air you inhale and exhale at rest. A healthy young adult has a tidal volume of about 500 milliliters, but the volume varies based on health, height, age, and sex. However, your lungs can hold a much larger volume of air called the vital capacity.
The vital capacity (VC) is the total volume of usable air.
Wait, don’t you mean vital essence?
No, the essence is what the Skeksis drink in the movie The Dark Crystal.

Oh, my bad. Can you give an example of vital capacity?
Sure. Inhale as much air as possible and then exhale until no air comes from your mouth. All the air you expire is your vital capacity.
Ok, I think I get it. However, is there a math equation that will help me quantify this concept?
Yes, there is. The formula for vital capacity (VC) is:
VC = inspiratory \: reserve \:volume + tidal\: volume + expiratory \: reserve \: volume
I like it. What is the inspiratory and expiratory reserve volume?
The inspiratory reserve volume (IRV) is the air you can inhale after inspiring your tidal volume.
Huh?
For example, inhale without effort and then forcefully inhale as much air as possible. The air that you force into your lungs is the IRV.
Oh. And the expiratory reserve volume?
The expiratory reserve volume (ERV) is the total air you exhale after your tidal volume. For example, expire a resting breath and then forcefully exhale as much air as possible. The air you force out of your lungs is the ERV.
So, the EDV is the opposite of the IDV?
Basically, yes.
So, when do I use my IRV and ERV?
You dip into your IRV and ERV when active because your body requires more oxygen.
I see. So, my vital capacity is the resting volume of inspired and expired air (tidal volume) plus my exercise volume (IRV and ERV).
Yep. However, about 1.2 liters of air, called the residual volume (RV), remains in your lungs after exhaling completely.
What?
The RV helps keep your alveoli inflated after you have released all of your ERV. If you have had the wind knocked out of you, you have experienced a partial loss of your residual volume. Impact on the medial ventral cavity can cause brief diaphragm paralysis and some RV loss. Normal respiration usually returns a few minutes after the impact.
So my lungs collapse when I get the wind knocked out of me?
No, getting the wind knocked out of you is not the same as a collapsed lung because the lungs do not collapse.
So, are there any other lung volumes?
The total lung capacity (TLC) is all the air in your lungs after a deep breath. The TLC is the sum of the IRV, tidal volume, ERV, and residual volume. The formula is:
Total \: Lung \: Capacity = Vital \: Capacity \: (IRV, tidal \: volume, and \: ERV) + residual \: volume

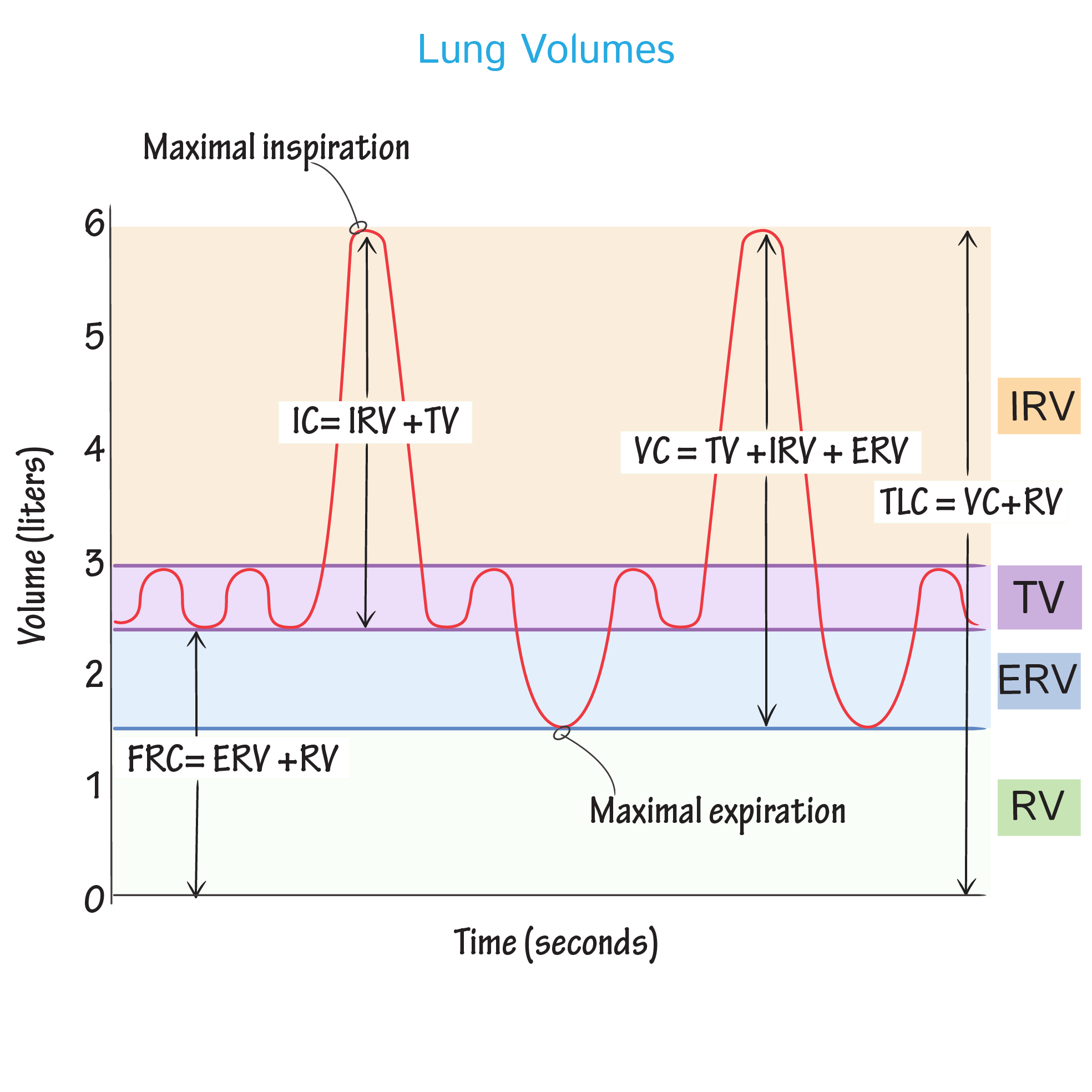
The functional residual capacity (FRC) is the air volume left in your lungs after a resting expiration. The inspiratory capacity (IC) is the maximum volume of air you can inspire.
Random Asthma Fact
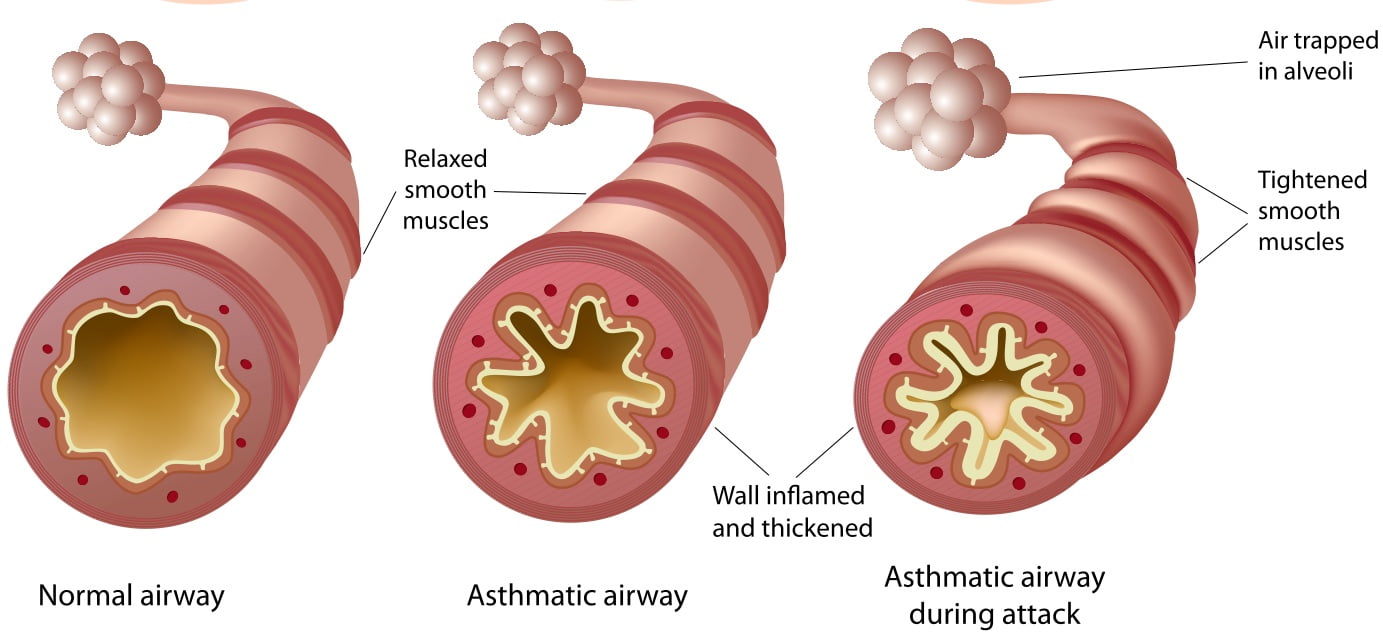
Unlike lung disease, asthma does not directly affect a person’s vital capacity. Asthma causes inflammation of the bronchial tubes, which decreases their diameter. Decreased bronchial diameter makes inspiration and expiration more difficult, reducing gas exchange. The exact cause of asthma is unknown, but exercise and/or allergens can lead to an asthma attack. Children who live in areas with poor air quality are more likely to have asthma attacks, and those with pets, especially dogs, are less likely to get asthma attacks.
External Respiration
The alveoli are tiny air sacs where gas exchange occurs. Simple squamous epithelium, or Type I cells, comprises the walls of the alveoli. The capillaries comprise simple squamous epithelium, too. Capillaries form a webbing around the alveoli, allowing quick and laborless gas exchange. Oxygen diffuses into the capillaries during inspiration, and carbon dioxide diffuses into the alveoli.


Scattered amid the type I cells are simple cuboidal type II cells. Type II cells secrete surfactant, which coats the gas-exposed alveolar surface. The role of surfactant is to reduce friction within the alveoli. Water is a polar molecule with high surface tension. Since water is the main component of the liquid film that coats the alveolar walls, its surface tension always reduces the alveoli to its smallest possible size. If the film were pure water, the alveoli would collapse between breaths.
I take it that collapsed alveoli are a bad thing.
Yep. Inflating the alveoli after each expiration would make breathing difficult.
So, how does surfactant prevent the alveoli from collapsing?
The surfactant in the alveolar film decreases the cohesiveness of the water. As a result, there is a decrease in the alveolar fluid’s surface tension, and less energy is needed to overcome those forces to expand the linings and discourage alveolar collapse.


Factors That Affect External Respiration
In a healthy lung, the alveoli have thin walls with high surface area, and the pulmonary capillaries tightly adhere to the alveolar walls. A diseased lung usually has one or more symptoms: reduced gas exchange rate, reduced surface area, thickening of the alveolar walls, and a barrier to the alveoli and the surrounding capillaries.

Vape Pen Lung Disease
Vape Pen Lung disease (VPLD) decreases the gas exchange between alveoli and pulmonary capillaries. The exact cause is still under study, but most evidence points to vitamin E acetate as the culprit. Vitamin E is an excellent skin moisturizer and essential nutritional vitamin; however, it should never enter your lungs. The leading hypothesis behind VPLD is that when vitamin E enters the lungs’ alveoli, it coats the walls and acts as a barrier that impedes gas exchange. The immune system responds, and the alveoli become inflamed, which decreases their surface area. When the lungs heal, scar tissue is added to the alveolar walls, thickening them. Therefore, the alveolar walls’ coating, inflammation, and thickening lead to decreased gas exchange. VPLD is an acute disorder that can reduce lung function and can lead to death within a few days, weeks, or months of vaping. By contrast, chronic lung diseases such as emphysema and lung cancer usually occur after decades of smoking cigarettes or marijuana.
Now, I’m not promoting smoking over vaping. Both are potentially lethal- i.e., every year, more people die from nicotine products than all other drugs combined. I am clarifying that vaping is NOT a healthier alternative to smoking. Both are addictive and deadly.
For more information on vaping and its effects on the lungs, click here, here, here, here, here, here, or here.

Internal Respiration
Most of the oxygen that enters the alveolar capillaries diffuses into erythrocytes (red blood cells) and binds to a hemoglobin protein. When oxygen binds to hemoglobin, it oxidizes the iron in hemoglobin, which turns the deep red deoxygenated erythrocyte (RBC) bright red. In a healthy adult, 98 to 100 percent of the RBCs, leaving the lungs, will be saturated with oxygen. Oxygen saturation below 90 percent indicates a decrease in healthy lung function with the need for medical intervention.
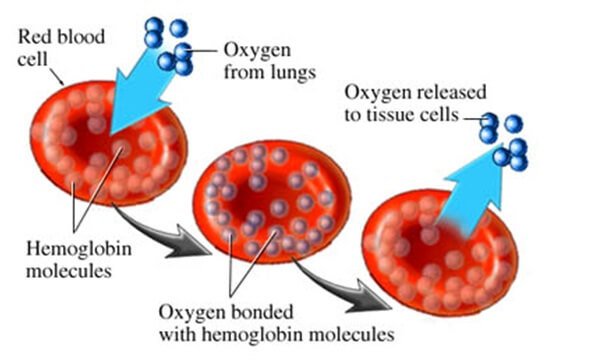
The oxygen-rich blood returns to the heart’s left side, and the left ventricle pumps the oxygen-saturated blood into the systemic arteries. The systemic arteries get smaller and smaller as they move away from the heart, eventually turning into arterioles, which then become capillaries. At the capillaries, the oxygen detaches from hemoglobin and diffuses into the cells of body tissues. The cells use oxygen to convert fat and glucose into ATP via cellular respiration. Cellular respiration produces carbon dioxide (CO2), a waste product. The CO2 diffuses into the blood, binds to hemoglobin, dissolves in the blood plasma, or becomes a bicarbonate ion (HCO3-).


The red blood cells convert 85% of the CO2 in the blood into HCO3–. The conversion of CO2 into HCO3- allows for (1) continual diffusion of CO2 into the blood and (2) helps maintain the slightly alkaline blood pH. HCO3– is the primary blood buffer that counteracts the hydrogen ions (H+) in the blood to keep blood pH in the homeostatic range of 7.35-7.45. Blood pH below 7.35 enters acidosis, and blood above 7.45 enters alkalosis. If the blood remains too acidic or basic, it can lead to organ failure and death.
The CO2-rich blood returns to the right side of the heart, and the right ventricle pumps the CO2-rich blood into the Pulmonary arteries. The pulmonary arteries become arterioles, the capillaries surrounding the alveoli. Plasma HCO3– converts to CO2, diffuses into the alveoli during external respiration, and leaves the lungs.
Chemistry is Fun!!!! Yes, it is.
Do you like chemistry? Who am I kidding? It’s the equivalent of 18 smartphones on top of a birthday cake. The figure to the right shows how most of the CO2 in blood transports to the lungs. So blow out the smartphones and learn about CO2 transport.
- CO2 produced during cellular respiration diffuses into the blood.
- Most CO2 diffuses into red blood cells (RBCs) and forms a bond with water, forming carbonic acid.
- Well, as you all know, carbonic acid is somewhat unstable, so it loses an H+ and becomes a bicarbonate ion (HCO3–).
- The HCO3– diffuses out of the RBC and enters the plasma, acting as a chemical buffer that helps maintain the blood pH at 7.4.
- When the blood enters the lung’s capillaries surrounding the alveoli, HCO3– reenters the RBC and converts back to carbonic acid, which then oxidizes into CO2 and water. The CO2 diffuses from the RBC into the plasma and then moves into the alveoli.
- Isn’t chemistry fun?!!!!!!

The result from the chest x-ray confirms that your patient has a tension pneumothorax. A tension pneumothorax happens with an object that punctures the cavity surrounding a lung called the pleural cavity. Usually, there is more pressure within the lungs than in the pleural cavity, which prevents the lung from collapsing during respiration. During a tension pneumothorax, the air entering the pleural cavity causes the pressure within said cavity to become greater than the lung’s pressure. The increase in pleural pressure causes the lung to collapse, affecting pulmonary ventilation, external respiration, and internal respiration. You place a patch over the hole in the thoracic wall and insert a percutaneous chest tube into the pleural space. The tube is a small, hollow needle with a valve on the end that remains outside the body. You open the valve, and air rushes out of the pleural cavity until the pressure within the cavity is less than the lungs. A few minutes later, the patient’s right lung inflates, and he begins to breathe normally. You clean and suture the knife wound.


Oxygen Consumption
VO2
Cells do not use all of the oxygen in the blood. The amount of oxygen consumed (VO2) is determined by our health, fitness, sex, and age. Healthier, younger people are more efficient at utilizing oxygen than older, unhealthy individuals. VO2 is in constant flux, so the body maintains a homeostatic level of oxygen usage. For example, your resting VO2 is less than your exercising VO2 because your muscles do not require as much oxygen at rest.
Is there a way to calculate the amount of oxygen a person consumes (VO2) using their CO?
Yep. The following is a basic, and I mean the basic, understanding of how CO can be used to determine VO2.
Example #1
Bob Bobby has a resting HR of 58 bpm and an SV of 103 ml/beat. What is his CO in ml/min?
\frac{53\:\bcancel{beats}}{minute}\times\:\frac{103\:ml}{\bcancel{beat}}\times\:\frac{1\:L}{\bcancel{1000\:ml}}=\colorbox{yellow}{5.5\:L/min}How much oxygen are Bob Bobby’s cells using per minute?
VO_2=CO\times\:0.05\:plasma\:O_2
5.5\:L/min\:x\:0.05\:plasma\:O_2=\colorbox{yellow}{0.275\:L/min \:or\:275\:ml/min}
Therefore, Bob Bobby’s cells consume 275 ml of oxygen gas per minute at rest. It is important to restate that VO2 is NOT the total amount of oxygen gas in the blood, but the amount of oxygen consumed by the body’s cells (About 25% of the blood oxygen is consumed, which means the blood in the veins contains about 75% the arterial oxygen. The high oxygen content of “deoxygenated” blood is why blood is still red, though deeper red).
VO2max
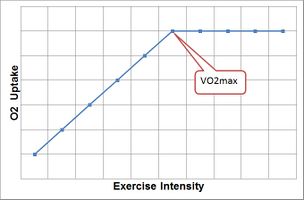
Your aerobic capacity, or VO2max, measures how efficiently you use the oxygen in your blood. VO2max is one measurement, not the only value, to determine fitness. People with a higher VO2max for their height, weight, age, and sex can better utilize blood oxygen than those with a lower VO2max with the same body variables.
VO2max is dependent on:
- Cardiac output
- Vital capacity
- Blood pressure
- Rate of oxygen delivery to muscle fibers and how efficiently muscles use said oxygen
There are multiple ways of measuring VO2max, but the most accurate way is to jog a mile constantly on a treadmill while wearing a mask that measures respired O2 and CO2. (You can use an exercise bike, too.) However, the technology required to measure respired O2 and CO2 is unavailable to most people. Some smartwatches will calculate VO2max, but the error rate can be over 30%. Comparing resting heart rate with the heart rate during exercise is the gold standard for those who do not have access to a machine that measures CO2 production and O2 consumption.
Heart rate is a good measurement of how well your cardiovascular and respiratory systems work and how well you use the oxygen in your blood. Healthier, fit individuals will have a lower resting heart rate and lower heart rate during exercise than a less fit individual doing the same activity at the same intensity. If you are like me and have not adequately exercised since the Truman Administration, you probably have a low VO2max. If you get about 150 minutes of exercise a week (the recommended minimum amount), you probably have a mid-range VO2max. If you exercise two or more hours daily, your VO2max is most likely in the high range.
| This is a Graph Showing VO2max | This is HBO Max |
|---|---|
 |  |
Example #2
Bob Bobby will jog a mile at a near-constant pace to measure his VO2max. He weighs 69.1 kg and has a resting HR of 53 bpm. It takes Bob Bobby 7 minutes and 15 seconds to jog the mile, and his heart rate is 153 bpm at the end of the jog. What is his VO2max?
Variables:
- Time = Time it takes to jog a mile, written in decimal form. For example, a time of 9 minutes and 30 seconds is written as 9.5
- HR = HR taken at the end of the one-mile jog
Females:\:VO_{2max}=\:100.5\:-\:[weight\:kg\:(0.1636)]\:-\:[time\:(1.438)]\:-\:[HR\:(0.1928)]Males:\:VO_{2max}=\:108.844\:-\:[weight\:kg\:(0.1636)]\:-\:[time\:(1.438)]\:-\:[HR\:(0.1928)]Bob\:Bobby's\:VO_{2max}=\:108.844\:-\:[69.1\:(0.1636)]\:-\:[7.25\:(1.438)]\:-\:[153\:(0.1928)]Bob\:Bobby's\:VO_{2max}=\:108.844\:-\:11.3\:-\:10.44\:-\:29.5Bob\:Bobby's\:VO_{2max}=\colorbox{yellow}{57.8\: ml/kg/min}Therefore, one kilogram of Bob Bobby’s cells can consume a maximum amount of 57.8 ml/min oxygen.
I hate running and moving. Is there a way I can calculate my VO2max without exercise?
Yes, but you should get at least 30 minutes of daily exercise.
Blinking winds me.
Oh. . . that’s not good.
I am getting mentally and physically tired from this conversation. I want a non-mile formula, please.
Example #3
Variables:
- HRrest = Resting heart rate
- HRmax = Heart rate a person should not exceed
VO_{2max}\:(ml/kg/min)=15.3\times\:\frac{HR_{max}}{HR_{rest}}First, you will need to calculate Bob Bobby’s HRmax. The formula is 220-age in years = HRmax. Bob Bobby is 23 years old.
220\:-\:23= \colorbox{yellow}{197\:bpm}Therefore, Bob Bobby’s HR should not exceed 197 bpm during exercise. Now that you have his HRrest (53 bpm) and HRmax, you can calculate his VO2max.
15.3\times\:\frac{197\:\bcancel{bpm}}{53\:\bcancel{bpm}}=\colorbox{yellow}{56.9\:ml/kg/min}